
GENEVA, Switzerland, August 23, 2024 (ENS) – The current mpox outbreak “can be controlled and can be stopped,” the leader of the World Health Organization, WHO, emphasized on Friday, announcing an action plan that calls for US$135 million over the next six months.
“Responding to this complex outbreak requires a comprehensive and coordinated international response,” WHO Director-General Tedros Adhanom Ghebreyesus told Member States, as cases spread beyond Africa to Europe and Asia.
The briefing was held just over a week after Dr. Tedros declared that mpox to be a public health emergency of international concern on August 14.
Africa Centers for Disease Control Director-General Jean Kaseya declared mpox to be a Public Health Emergency of Continental Security on August 13.
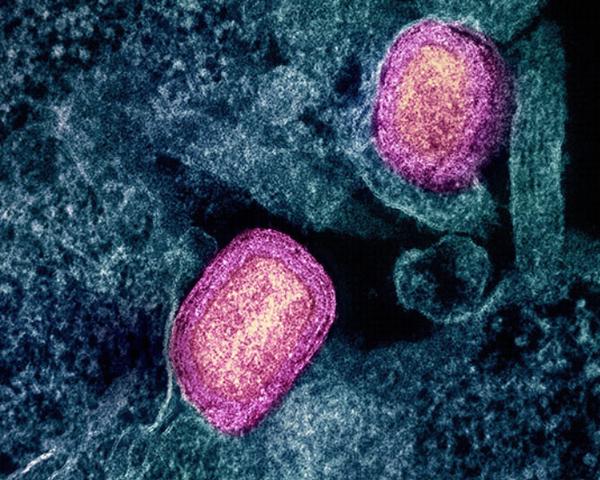
New Mpox Virus Strain Appears
Dr. Tedros said the global outbreak first emerged in 2022, with more than 100,000 confirmed cases reported since then. While the virus continues to circulate at low levels, Africa has seen an unprecedented increase and expansion.
Transmission is mainly centered in the Democratic Republic of the Congo, DRC, where there have been more than 16,000 suspected cases, including 575 deaths, this year alone.
What WHO calls “the surge” is being driven by two separate outbreaks of two strains, or clades, of the mpox virus in different parts of the country.
The rapid spread of a new offshoot, clade 1b, was the main reason behind Dr. Tedros’ decision to declare mpox a global public health emergency on August 14, WHO said in a statement.
“In the past month, cases of clade 1b have been reported in four countries neighboring DRC, which had not reported mpox before: Burundi, Kenya, Rwanda and Uganda. This week, cases have also been reported in Thailand and Sweden,” said Dr. Tedros, who holds a PhD in community health from the University of Nottingham.
Four nations: Pakistan, Philippines, Sweden, and Thailand, have reported mpox cases outside the African continent, while 14 countries within Africa have reported cases.
Mpox, a New Name for a Decades-Old Disease
Monkeypox, now called mpox, got its name in 1958, when it was detected in several laboratory apes. It is a zoonotic viral disease, it can be transmitted from animals to humans and also from human to human.
Human monkeypox was first identified in 1970 in the Democratic Republic of the Congo (DRC) in a nine-month-old boy, in a region where smallpox, a close relative of mpox, had been eliminated in 1968.
Symptoms are similar to those seen, in the past in smallpox patients, but it is clinically less severe; smallpox was eradicated worldwide in 1980.
In 2003, the first monkeypox outbreak outside Africa was reported in the United States and was linked to contact with infected pet prairie dogs.
Despite the name, most of the animals susceptible to contracting the disease, and then infecting people, are not monkeys but rodents, such as Gambian giant rats, dormice, or tree squirrels.
Mpox, as it is now more accurately called, is most found in the rain forests of central and western Africa, where animals that can carry the virus are native, and the disease is endemic. In these countries, it is increasingly found in urban areas.
Sometimes mpox can be found elsewhere, in people who could have been infected after visiting these countries.
Symptoms usually include fever, severe headache, muscle aches, back pain, low energy, swollen lymph nodes, and skin rashes or lesions.
In most cases, the symptoms of mpox go away on their own within a few weeks but, in between three and six percent of cases reported in countries where it is endemic, it can lead to medical complications and even death. New-born babies, children, and people with immune system deficiencies may be at risk of more severe symptoms and death from the disease.
Mpox Can Be Stopped, WHO Chief Believes
WHO and its partners have developed a plan to stop outbreaks of human-to-human transmission of mpox through coordinated efforts at the global, regional, and national levels.
“Let me be clear: this new mpox outbreak can be controlled and can be stopped,” Dr. Tedros asserted.
“Doing so requires concerted action between international agencies and national and local partners, civil society, researchers and manufacturers, and you, our Member States,” he said.
He stressed that response must be anchored in “equity, global solidarity, community empowerment, human rights, and coordination across sectors.”
Response Emphasizes Leadership, Preparedness, Coordination
The Global Mpox Strategic Preparedness and Response Plan, SPRP, focuses on comprehensive surveillance and response strategies, and advancing research and equitable access to medical countermeasures.

“Our initial estimates are that the SPRP requires approximately $135 million over the next six months for the acute phase of the outbreak. That amount will likely increase as we update the plan in light of growing needs,” Tedros said. A dedicated WHO funding appeal will be issued early next week.
The Mpox Strategic Plan calls for minimizing zoonotic transmission from animals to humans and empowering communities to actively participate in outbreak prevention and control.
At the global level, emphasis is on strategic leadership, timely evidence-based guidance, and access to medical countermeasures for the most at-risk groups in affected countries.
WHO is working with a range of international, regional, national and local partners and networks to enhance coordination across the key areas of preparedness, readiness and response.
WHO regional offices have established Incident Management Support Teams to lead preparedness and response activities, while staffing is being scaled up in affected countries.
Preventing Transmission Saves Lives
The Regional Office for Africa, in collaboration with the African Centres for Disease Control, will jointly spearhead the coordination of mpox response efforts, given that needs on the African continent are greatest.
Meanwhile, health authorities at the national and sub-national levels will adapt strategies to current epidemiological trends.
There is no treatment for mpox currently. However, there is an mpox vaccine that can be taken to prevent infection. The vaccine most commonly used for preventing mpox is JYNNEOS, also called Imvamune or Imvanex, which has been licensed by the U.S. Food and Drug Administration.
Scientists also are working with smallpox vaccines. ACAM2000® is the primary smallpox vaccine designated for use in a bioterrorism emergency, with doses supplied to the U.S. Strategic National Stockpile. ACAM2000® is also licensed in Canada, Australia, and Singapore and is currently stockpiled both in the United States and internationally.
Dr. Tedros noted that WHO has so far released approximately US$1.5 million from an emergency fund, with more allocations expected in the coming days, “until funding from donors for the response comes in.”
He said WHO “will coordinate the global response, working closely with each of the affected countries, to prevent transmission, treat those infected, and save lives.”
Featured image: WHO Director-General Tedros Adhanom Ghebreyesus, PhD speaks at the opening of the 10th meeting of the Intergovernmental Negotiating Body for a WHO instrument on pandemic prevention, preparedness and response, July 16, 2024, WHO Headquarters, Geneva, Switzerland (Photo © WHO / Lindsay Mackenzie)
© 2024, Environment News Service. All rights reserved. Content may be quoted only with proper attribution and a direct link to the original article. Full reproduction is prohibited.



