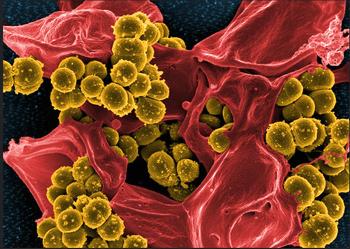
ARLINGTON, Virginia, January 9, 2017 (ENS) – The Department of Veterans Affairs’ eight-year-long campaign to limit the incidence of infections with the dangerous methicillin-resistant Staphylococcus aureus, or MRSA, in VA healthcare facilities continues to make progress, a new study shows.
MRSA causes a range of serious illnesses, from skin and wound infections to pneumonia and bloodstream infections that can lead to sepsis and death.
Staph bacteria, including MRSA, are one of the most common causes of healthcare-associated infections.
Martin E. Evans, MD, and colleagues from the Veterans Health Administration, found that between October 2007 and September 2015 monthly rates of hospital acquired infections dropped 87 percent in intensive care units, ICUs; 80.1 percent in non-ICUs; and 80.9 percent in spinal cord injury units.
In long-term care facilities, rates fell 49.4 percent during the period of July 2009 to September 2015.
“Understanding how and why rates of MRSA have diminished in recent years is essential for the continued progress of effective prevention programs,” said Dr. Evans.
Nationwide, in September 2015, only two MRSA infections in healthcare facilities were reported in Intensive Care Units, 20 in non-ICUs, and 31 in long-term care facilities.
“As we seek to protect patients from MRSA and other resistant organisms, our study supports the need for strong infection prevention programs at every healthcare facility,” Evans said.
Prior to 2007, rates of MRSA infection in Veterans Administration health care facities were what the VA determined were “unacceptably high.” This led the vetrans agency to implement the MRSA Prevention Initiative nationwide in October 2007.
A previous study published by the same researchers shows a decline in MRSA transmissions and MRSA in health care facilitiess between October 2007 and June 2012 in acute care medical centers, between October 2007 and June 2011 in spineal cord units, and between July 2009 and December 2012 in long-term care facilities, giving some indication that the initiative was working.
The current study updates and supports these continuing trends in MRSA transmission and exposure in hospitals through September 2015, an eight-year study period.
The VA program placed a dedicated MRSA prevention coordinator at each healthcare facility to oversee a host of interventions including: universal active screening on admission, unit-to-unit transfer, and discharge; contact precautions for those colonized or infected with MRSA; adherence to hand hygiene; and institutional culture change where infection prevention became everyone’s business.

The study is published in the January issue of the “American Journal of Infection Control,” the official journal of the Association for Professionals in Infection Control and Epidemiology.
The authors speculate that the focused attention on MRSA infections helped motivate healthcare workers to practice better infection prevention and control measures.
“We speculate that active surveillance was the primary driver of the downward trends seen in the VA,” said Evans, noting that the rates of MRSA in health care facilities had not changed before October 2007 when the initiative was fully implemented.
Formal recommendations for hand hygiene and device-related infection control had been in place for several years by then.
Attention to hygiene is a good idea in all situations. Studies show that 33 percent of people carry staph in their nose, usually without any illness, while two out of 100 people carry MRSA, according to the Centers for Disease Control and Prevention.
“The discovery, development and deployment of antibiotics have transformed medicine; however, microbes continually evolve and become resistant to these lifesaving drugs,” said Anthony Fauci, M.D., director of the National Institute of Allergy and Infectious Diseases, NIAID, part of the National Institutes of Health.
“New strategies are desperately needed to treat patients with antibiotic-resistant infections that often are deadly, Dr. Fauci said, announcing the recipients of about $5 million in grants for research into non-traditional therapies that could complement or even replace currently available antibiotics that are losing effectiveness.
Copyright Environment News Service (ENS) 2017. All rights reserved.
