ST. LOUIS, Missouri, November 29, 2021 (ENS) – Lasers that emit ultrashort pulses of light can kill multidrug-resistant bacteria such as MRSA and E. coli, researchers at Washington University School of Medicine in St. Louis have discovered.
Life-threatening bacteria are becoming ever more resistant to antibiotics, making the search for alternatives to antibiotics an urgent challenge. One possibility appears to be this unique type of laser. It does not destroy all such bacteria, but for some applications, ultrashort-pulse lasers are just what’s needed.
The study, online in the “Journal of Biophotonics,” opens the possibility of using ultrashort-pulse lasers to destroy bacteria that are hard to kill by other methods.
The same group of researchers previously had shown that such lasers don’t damage human cells, making it possible to use the lasers to sterilize wounds or disinfect blood products.
“The ultrashort-pulse laser technology uniquely inactivates pathogens while preserving human proteins and cells,” said first author Shaw-Wei “David” Tsen, MD, PhD, an instructor of radiology at Washington University’s Mallinckrodt Institute of Radiology (MIR).
“Imagine if, prior to closing a surgical wound, we could scan a laser beam across the site and further reduce the chances of infection. I can see this technology being used soon to disinfect biological products in vitro, and even to treat bloodstream infections in the future by putting patients on dialysis and passing the blood through a laser treatment device.”
Tsen and senior author Samuel Achilefu, PhD, professor of radiology and director of MIR’s Biophotonics Research Center, have been exploring the germicidal properties of ultrashort-pulse lasers for years. They have shown that such lasers can inactivate viruses and ordinary bacteria without harming human cells.
In the new study, they collaborated with Shelley Haydel, PhD, a professor of microbiology at Arizona State University, extending their exploration to antibiotic-resistant bacteria and bacterial spores.
The researchers trained their lasers on multidrug-resistant Staphylococcus aureus, MRSA, which can cause dangerous or even deadly infections of the skin, lungs and other organs.
In healthcare facilities such as hospitals and nursing homes, the patients or residents most likely to get an MRSA infection are those with other health conditions making them sick, according to the Centers for Disease Control and Prevention, CDC. Also, hospital or nursing home patients who have been treated with antibiotics, have wounds or invasive medical devices such as catheters, or have certain procedures like surgery or dialysis are more likely to get an infection.
The researchers also worked with extended spectrum beta-lactamase-producing Escherichia coli, E. coli, a large and diverse group of bacteria found in the environment, foods, and intestines of people and animals.
Most strains of E. coli are harmless, but others can cause urinary tract infections, diarrhea, respiratory illness and pneumonia, and other illnesses.
MRSA and E. coli are entirely different types of bacteria, from two distant branches of the bacterial kingdom.
The researchers also investigated spores of the bacterium Bacillus cereus, which causes food poisoning and food spoilage. Bacillus spores can withstand boiling and cooking.
In all these cases, the ultrashort-pulse lasers killed more than 99.9 percent of the target organisms, reducing their numbers by more than 1,000 times.
How It Works
Viruses and bacteria contain densely packed protein structures that can be excited by an ultrashort-pulse laser. The Washington University School of Medicine research team explains that the laser kills by causing these protein structures to vibrate until some of their molecular bonds break.
The broken ends quickly reattach to whatever they can find, which in many cases is not what they had been attached to before. The result is a mess of incorrect linkages inside and between proteins, and that mess causes normal protein function in microorganisms to grind to a halt.
But passing the ultrashort-pulse laser through human tissue does not create a mess, it kills no human cells, the researchers have shown.
“We previously published a paper in which we showed that the laser power matters,” Tsen said. “At a certain laser power, we’re inactivating viruses. As you increase the power, you start inactivating bacteria. But it takes even higher power than that, and we’re talking orders of magnitude, to start killing human cells. So there is a therapeutic window where we can tune the laser parameters such that we can kill pathogens without affecting the human cells.”
Heat, radiation and chemicals such as bleach are effective at sterilizing objects, but most of these methods are too damaging to be used on people or biological products. By inactivating all kinds of bacteria and viruses without damaging cells, ultrashort-pulse lasers could provide a new approach to making blood products and other biological products safer.
“Anything derived from human or animal sources could be contaminated with pathogens,” Tsen said. “We screen all blood products before transfusing them to patients. The problem is that we have to know what we’re screening for. If a new blood-borne virus emerges, like HIV did in the ’70s and ’80s, it could get into the blood supply before we know it.”
Tsen said, “Ultrashort-pulse lasers could be a way to make sure that our blood supply is clear of pathogens both known and unknown.”
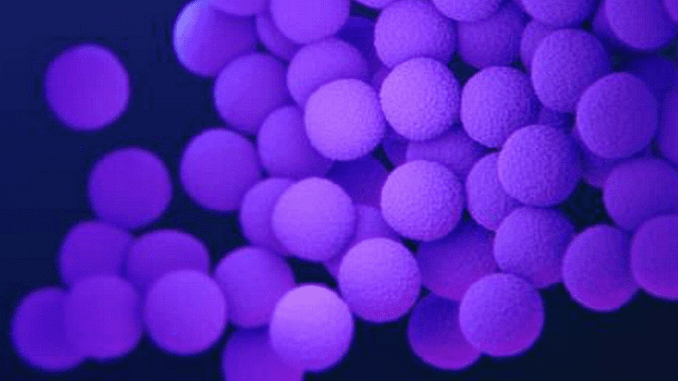
Featured image: A medical illustration of methicillin-resistant, Staphylococcus aureus, MRSA, bacteria, presented in the Centers for Disease Control and Prevention, CDC, publication “Antibiotic Resistance Threats in the United States, 2019.”
© 2021, Environment News Service. All rights reserved. Content may be quoted only with proper attribution and a direct link to the original article. Full reproduction is prohibited.


