ATLANTA, Georgia, March 5, 2013 (ENS) – Drug-resistant germs called carbapenem-resistant Enterobacteriaceae, or CRE, are on the rise and have become more resistant to last-resort antibiotics over the past decade, warns a new report from the Centers for Disease Control and Prevention.
These bacteria are causing more hospitalized patients to get infections that, in some cases, are impossible to treat, warns the CDC Vital Signs report for March 2013, issued today.
“CRE are nightmare bacteria. Our strongest antibiotics don’t work and patients are left with potentially untreatable infections,” said CDC Director Tom Frieden, M.D., M.P.H. “Doctors, hospital leaders, and public health, must work together now to implement CDC’s “detect and protect” strategy and stop these infections from spreading.”
CRE are lethal bacteria that pose a triple threat:
- Resistance: CRE are resistant to all, or nearly all, known antibiotics – even the most powerful drugs of last resort.
- Death: CRE have high mortality rates. CRE germs kill half of all patients who get bloodstream infections from them.
- Spread of disease: CRE easily transfer their antibiotic resistance to other bacteria. For example, carbapenem-resistant klebsiella can spread its drug-destroying weapons to a normal E. coli bacteria, which makes the E.coli resistant to antibiotics also. That could create a nightmare scenario since E. coli is the most common cause of urinary tract infections in healthy people.
Currently, almost all CRE infections occur in people receiving major medical care, such as long-term care, dialysis, those who have medical devices such as catheters, and people who have had surgery within the past year.

CRE are usually transmitted from person-to-person, often on the hands of health care workers.
Enterobacteriaceae are a family of more than 70 bacteria including Klebsiella pneumoniae and E. coli that normally live in the digestive system. Over time, some of these bacteria have become resistant to a group of antibiotics known as carbapenems, often referred to as last-resort antibiotics.
During the last decade, CDC has tracked one type of CRE from a single health care facility to health care facilities in at least 42 states. In some medical facilities, these bacteria already pose a routine challenge to health care professionals.
In 2012, the Centers for Disease Control released a concise, practical CRE prevention toolkit with in-depth recommendations to control CRE transmission in hospitals, long-term acute care facilities, and nursing homes.
“We have seen in outbreak after outbreak that when facilities and regions follow CDC’s prevention guidelines, CRE can be controlled and even stopped,” said Michael Bell, M.D., acting director of CDC’s Division of Healthcare Quality Promotion. “As trusted health care providers, it is our responsibility to prevent further spread of these deadly bacteria.”
Key recommendations include:
- enforcing use of infection control precautions
- grouping patients with CRE together
- dedicating staff, rooms and equipment to the care of patients with CRE whenever possible
- having facilities alert each other when patients with CRE transfer back and forth
- asking patients whether they have recently received care somewhere else, including another country
- using antibiotics wisely
In addition, CDC recommends screening patients in certain scenarios to determine if they are carrying CRE. Because of the way CRE can be carried by patients from one health care setting to another, facilities are encouraged to work together regionally to implement CRE prevention programs.
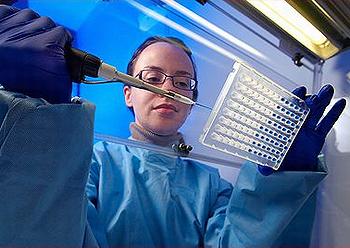
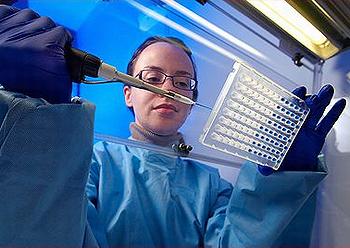
These core prevention measures are critical and can significantly reduce the problem today and for the future, says the CDC. In addition, continued investment into research and technology, such as a testing approach called Advanced Molecular Detection, is critical to further prevent and more quickly identify CRE.
In some parts of the world, CRE appear to be more common, and evidence shows they can be controlled.
Israel recently employed a coordinated effort in its 27 hospitals and dropped CRE rates by more than 70 percent. Several facilities and states in the U.S. have also seen similar reductions.
In the latest study tracking CRE, out of the total of 3,918 hospitals reporting during the first six months of 2012, the long-term acute-care hospitals has the greatest percentage of CRE appearances.
Of the 212 total long-term acute-care hospitals reporting, 36 had at least one case of CRE.
Of the short-stay hospitals reporting, 145 had at least one case of CRE.
Study co-author Alexander Kallen of the CDC told ENS in an interview, “The important message here is that, although these bacteria are becoming more common, most hospitals don’t see these on a regular basis. We still have the opportunity to intervene. When you think of other bugs like MRSA [Methicillin-resistant Staphylococcus aureus], we haven’t reached that stage with this bacteria.”
© 2013, Environment News Service. All rights reserved. Content may be quoted only with proper attribution and a direct link to the original article. Full reproduction is prohibited.
